Carbapenem Resistant Gram-Negative Organisms: Therapeutic Options In A Resource Limited Setting
Main Article Content
Abstract
Introduction: Health care associated infections due to carbapenem resistant gram-negative bacteria (CRGNB) are on the rise with limited available therapeutic options for these infections. Therapeutic options include newer drugs and drug combinations, which are not readily accessible in low resource. Older more affordable drugs have been reported to have good antimicrobial activity against some of these pathogens. This study aimed to determine the susceptibility profile of CRGNB isolates to the recommended, readily available and affordable, antibiotics in our setting.
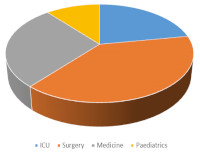
Methods: This cross-sectional laboratory-based study was carried out from December 2017-August 2018. Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa and Acinetobacter baumannii identified from inpatient specimens were subjected to susceptibility testing using the modified Kirby- Bauer technique. Carbapenem resistant isolates were further subjected to susceptibility tests against tigecycline, colistin, fosfomycin, polymyxin B, amikacin, and piperacillin-tazobactam. Breakpoints were read off using CLSI standards and appropriate controls.
Results: Of the 238 isolates studied, 18 (8.2%) showed resistance to ertapenem while 16 (6.7%) and 15 (6.3%) showed resistance to imipenem and meropenem respectively. Tigecycline, colistin, and polymyxin B showed impressive activity 94%, 88% and 83% activity against carbapenem resistant organisms respectively.
Conclusion: Tigecycline, colistin and polymyxin B are effective therapeutic options for treatment of infections caused by CRGNB. To optimize clinical improvement and reduce morbidity and mortality associated with these infections in resource poor countries, we recommend the use of tigecycline, colistin or polymyxin B for empirical treatment of infections caused by these pathogens.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
Share
References
Trecarichi EM, Tumbarello M. Therapeutic options for carbapenem-resistant. Virulence. 2017;8(4): 470–484
Jesumirhewe C, Springer B, Lepuschitz S, Allerberger F, Ruppitsch W. Carbapenemase-producing Entero bacteria ceae isolates from Edo State, Nigeria. Antimicrobial Agents Chemotherapy. 2017; 61:e00255-17
Nordmann P, Dortet L, Poirel L “Carbapenem resistance in enterobacteriaceae: here is the storm”. Trends in molecular medicine. 2012; 18(5): 263-273.
Sacha P, Ostas A, Jaworowska J, Wieczorek P, Ojdana D, Ratajczak J.et.al; The KPC type beta-lactamases: New enzymes that confer resistance to carbapenemen in Gramnegative bacilli. Folia Histochemica et Cytobiologica. 2009;47(4): 537-543.
Brennan-Krohn T, ManetschRO'Doherty GA, Kirby JE. New Strategies and Structural considerations in Development of Therapeutics for Carbapenem-Resistant Enterobacteriaceae: New Therapies for CRE. Translational Research.2020 [accessed 2020 June 20]. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC 7293594. Doi 10.1016/j.trsl.2020.02.008.
Perez F, El-Chakhtoura NG, Papp-Wallace KM, Wilson BM, Bonomo RA. Treatment options for infections caused by carbapenem-resistant Enterobacteriaceae: can we apply “precision medicine” to antimicrobial chemotherapy. Expert opinion on pharmacotherapy. 2016 ;17(6):761-81.
Sheu CC, Chang YT, Lin SY, Chen YH, Hsueh PR. Infections Caused by Carbapenem-Resistant Enterobacteriaceae: An Update on Therapeutic Options. Front. Microbiol. 2019 [ accessed 2020 July 5]; 10:80. doi: 10.3389/fmicb.2019.00080.
Petty LA, Henig, O, Patel TS, Pogue JM, Kaye KS. Overview of meropenem-vaborbactam and newer antimicrobial agents for the treatment of carbapenemresistant Enterobacteriaceae. Infect. Drug Resist [Internet] . 2018 [accessed 2020 June 20]; 11: 1461–1472. doi: 10.2147/IDR.S150447
Willyard, C. The drug-resistant bacteria that pose the greatest health threats. Nature [Internet]. 2017 [accessed 2020 June 20], 543:15. doi: 10.1038/nature.2017.21550
Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, 2013. Atlanta: CDC, 2014 [accessed 2018 July 26] Available at: http://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. 27th ed. CLSI supplement M100-S28. Clinical and Laboratory Standards Institute, Wayne, PA. 2018
European committee on antimicrobial susceptibility testing. Breakpoints for interpretation of MICs and zone diameters version 9.0 2019
Garg A, Garg J, Kumar S, Bhattacharya A, Agarwal S, Upadhyay GC. Molecular epidemiology& therapeutic options of carbapenem-resistant Gram-negative bacteria. The Indian Journal of Medical Research. 2019 ;149 (2):285.
Lee GC, Burgess DS. Treatment of Klebsiella pneumoniae carbapenemases (KPC) infection; a review of published case series and case reports. Ann Clin Microbiol, Antimicrob. [Internet] 2012 [accessed 2018 Aug 13] ; 11; 32,102-111. Available at doi: 10.1186/1476-0711-11-32.
Greer ND. Tigecycline (Tygacil): the first in the glycylcycline class of antibiotics. Proc BaylUniv Med Cent. 2006; 19:2,155–161.
Garrison MW, Neumiller JJ, Setter SM. Tigecycline: an investigational glycylcycline antimicrobial with activity against resistant gram-positiveOrganisms. Clinical Therapeutics. 2005;27(1):12–22.
Tumbarello M, Trecarichi EM, De Rosa FG, Giannella M, Giacobbe DR, BassettiM, et al. Infections caused by KPC producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. Journal of Antimicrobial Chemotherapy .2015; 70(7):2133-43.
Capone A, Giannella M, Fortini D, Giordano A, Meledandri M, Ballardini M, et al. High rate of colistin resistance among patients with carbapenem-resistant Klebsiella pneumoniae infection accounts for an excess of mortality. Clinical Microbiology and Infection. 2013; 19(1):E23-30; PMID: 23137235;
Pantović V, Dinić M, Stanković-Đorđević D, Kocić B, Bogdanović M. Susceptibility pattern of carbapenem resistant clinical isolates of Acinetobacter spp. Acta Medica Medianae. 2016; 55 (4):86-91.
Poirel L, Jayol A, Nordmann P. Polymyxins: antibacterial activity, susceptibility testing, and resistance mechanisms encoded by plasmids or chromosomes. Clinical Microbiology Reviews. 2017 [accessed 2020 June 6], 30:557–596. doi.10.1128/ CMR.00064-16.
Garonzik SM, Li J, Thamlikitkul V, Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrobial Agents Chemotherapy.2011; 55:3284–94.