Sociodemographic and Clinical Determinants of Adherence to Blood Pressure medication in hypertensive subjects.
Main Article Content
Abstract
Background. Blood pressure control in hypertension reduces cardiovascular disease morbidity and mortality. A significant factor that may contribute to blood pressure control is medication adherence. The aim of this study was to determine the sociodemographic and clinical factors that influence adherence to antihypertensive medication in hypertensive patients in Port Harcourt, Nigeria.
Methods. This was a descriptive cross-sectional study conducted in the cardiology clinics of Rivers State University Teaching Hospital and University of Port Harcourt Teaching Hospital. A total of 426 previously diagnosed hypertensive subjects on follow up for at least 6 months were assessed. Medication adherence was assessed using the Morisky's Medication Adherence Scale-8 with a score>/=3 indicative of nonadherence to medication. Data was analyzed using statistical software package SPSS version 22. Bivariate logistic regression analysis was used to identify factors influencing adherence to anti-hypertensive medications.
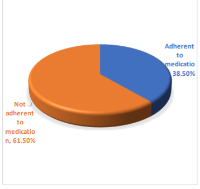
Results. The mean age of the respondents was 57.89+/-12.17years and 237(55.6%) were women. A total of 262(61.5%) respondents were not adherent to their medication while 164(38.5%) reported good medication adherence and the most frequent self reported reason for poor adherence was "I only take them when I have symptoms I attribute to hypertension" in 148(34.8%) persons. Significant predictors of medication nonadherence were age group (p<0.001), marital status (p<0.001), educational level (p<0.001), absence of comorbidities (p<0.001), and absence of complications of hypertension (p=0.001).
Conclusion. Adherence to antihypertensive medication in this study was poor, therefore, continuous adherence counselling should be encouraged in hypertensive patients with these identified factors to improve adherence, blood pressure control and ultimately, cardiovascular outcomes.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
How to Cite
Share
References
James PA, Oparil S, Carter BL, Cushman WC, DennisonHimmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC. 2014 evidencebased guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). Jama. 2014 Feb 5;311(5):507-20.
Schwartz JK, Aylmer K, Green S, Tayeb S, Wolf TJ, Unni E, Somerville E. Performance of Medication Tasks: Relationship Among Patient-Reported Outcomes, Performance-Based Assessments, and Objective Assessments. The American Journal of Occupational Therapy. 2024 May 1;78(3).
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016 Aug 9;134(6):441-50.
Wright Jr JT, Whelton PK, Johnson KC, Snyder JK, Reboussin DM, Cushman WC, Williamson JD, Pajewski NM, Cheung AK, Lewis CE, Oparil S. SPRINT revisited: updated results and implications. Hypertension. 2021 Dec;78(6):1701-10.
Schiffrin EL. The year in clinical hypertension from other pages. American Journal of Hypertension. 2018 Jan 12;31(2):136-8.
Burnier M, Egan BM. Adherence in hypertension: a review of prevalence, risk factors, impact, and management. Circulation research. 2019 Mar
;124(7):1124-40.
Oyan B, Abere S, Nwazor EO, Ajala AO, Briggs FK, Iroegbu-Emeruem L. Blood Pressure Control and Its Determinants Among Outpatient Hypertensive Subjects in Port Harcourt: A Survey of Two Teaching Hospitals. Journal of Advances in Medical and Pharmaceutical Sciences. 2024 Feb 27;26(4):14-23.
Hamrahian SM, Maarouf OH, Fülöp T. A critical review of medication adherence in hypertension: barriers and facilitators clinicians should consider. Patient preference and adherence. 2022 Jan 1:2749-57.
Walther D, Curjuric I, Dratva J, Schaffner E, Quinto C, Rochat T, Gaspoz JM, Burdet L, Bridevaux PO, Pons M, Gerbase MW. High blood pressure: prevalence and adherence to guidelines in a population-based cohort. Swiss medical weekly. 2016;146:w14323.
Oung AB, Kosirog E, Chavez B, Brunner J, Saseen JJ. Evaluation of medication adherence in chronic disease at a federally qualified health center. Therapeutic advances in chronic disease. 2017 Aug;8(8-9):113-20.
Mancia G, Zambon A, Soranna D, Merlino L, Corrao G. Factors involved in the discontinuation of antihypertensive drug therapy: an analysis from real life data. Journal of hypertension. 2014 Aug 1;32(8):1708- 16.
Mekonnen HS, Gebrie MH, Eyasu KH, Gelagay AA. Drug adherence for antihypertensive medications and its determinants among adult hypertensive patients attending in chronic clinics of referral hospitals in Northwest Ethiopia. BMC Pharmacology and Toxicology. 2017 Dec;18:1-0.
Guglielmi M, De Matteis C, Favale S, Manfellotto D, Taddei S, Scalvini S, Rosei EA, Palatini P, Villa G, Destro M, Venco A. Blood pressure control and treatment adherence in hypertensive patients with metabolic syndrome: protocol of a randomized controlled study based on home blood pressure telemonitoring vs. conventional management and assessment of psychological determinants of adherence (TELEBPMET Study).
Lee H, Yano Y, Cho SM, Heo JE, Kim DW, Park S, Lloyd-Jones DM, Kim HC. Adherence to antihypertensive medication and incident cardiovascular events in young adults with hypertension. Hypertension. 2021 Apr;77(4):1341-9.
Frias J, Virdi N, Raja P, Kim Y, Savage G, Osterberg L. Effectiveness of digital medicines to improve clinical outcomes in patients with uncontrolled hypertension and type 2 diabetes: prospective, open-label, clusterrandomized pilot clinical trial. Journal of medical Internet research. 2017 Jul 11;19(7):e246.
Pristianty L, Hingis ES, Priyandani Y, Rahem A. Relationship between knowledge and adherence to hypertension treatment. Journal of public health in Africa. 2023 Mar 3;14(Suppl 1).
Velázquez Fuentes MN, Shah P, Hale GM. Improving medication adherence in patients with hypertension through pharmacist-led telehealth services. Journal of Telemedicine and Telecare. 2022 Sep;28(8):613-7.
Morisky DE, Ang A, Krousel‐Wood M, Ward HJ. Retracted: predictive validity of a medication adherence measure in an outpatient setting. The journal of clinical hypertension. 2008 May;10(5):348-54.
Charchar FJ, Prestes PR, Mills C, Ching SM, Neupane D, Marques FZ, Sharman JE, Vogt L, Burrell LM, Korostovtseva L, Zec M. Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. Journal of hypertension. 2024 Jan 1;42(1):23-49.
Bergland OU, Halvorsen LV, Søraas CL, Hjørnholm U, Kjær VN, Rognstad S, Brobak KM, Aune A, Olsen E, Fauchald YM, Heimark S. Detection of nonadherence to antihypertensive treatment by measurements of serum drug concentrations. Hypertension. 2021 Sep;78(3):617- 28.
Osula D, Wu B, Schesing K, Das SR, Moss E, Alvarez K, Clark C, Halm EA, Brown NJ, Vongpatanasin W. Comparison of pharmacy refill data with chemical adherence testing in assessing medication nonadherence in a safety net hospital setting. Journal of the American Heart Association. 2022 Oct 4;11(19):e027099.
Thirunavukkarasu A, Naser Abdullah Alshahrani A, Mazen Abdel-Salam D, Homoud Al-Hazmi A, Farhan ALruwaili B, Awad Alsaidan A, Narapureddy BR, Muteb AL-Ruwaili A, Ghuwayli aljabri F, Khalaf Albalawi R, Alanazi KA. Medication adherence among hypertensive patients attending different primary health centers in Abha, Saudi Arabia: a cross-sectional study. Patient preference and adherence. 2022 Jan 1:2835-44.
Asgedom SW, Atey TM, Desse TA. Antihypertensive medication adherence and associated factors among adult hypertensive patients at Jimma University Specialized Hospital, southwest Ethiopia. BMC research notes. 2018 Dec;11:1-8.
Hussein A, Awad MS, Mahmoud HE. Patient adherence to antihypertensive medications in upper Egypt: a crosssectional study. The Egyptian Heart Journal. 2020 Dec;72:1-8.
Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs: a systematic review and metaanalysis. Medicine. 2017 Jan 1;96(4):e5641.
Adisa R, Ilesanmi OA, Fakeye TO. Treatment adherence and blood pressure outcome among hypertensive outpatients in two tertiary hospitals in Sokoto, Northwestern Nigeria. BMC cardiovascular disorders. 2018 Dec;18:1- 0.
Adeoye AM, Adebiyi AO, Adebayo OM, Owolabi MO. Medication adherence and 24-h blood pressure in apparently uncontrolled hypertensive Nigerian patients. Nigerian postgraduate medical journal. 2019 Jan 1;26(1):18-24.
Kretchy IA, Owusu-Daaku FT, Danquah S. Locus of control and anti-hypertensive medication adherence in Ghana. The Pan African Medical Journal. 2014;17(Suppl 1).
Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. Cmaj. 1999 Jan 12;160(1):31-7.
Svensson S, Kjellgren KI, Ahlner J, Säljö R. Reasons for adherence with antihypertensive medication. International journal of cardiology. 2000 Nov 1;76(2- 3):157-63.
Kramoh KE, Terline D, Macquart D, Damourou JM, Kouam CK, Toure IA, Mipinda JB, Diop BI, Ferreira B, Houenassi MD, Kuate LM. Factors associated with poor adherence to medication among hypertensive patients in twelve low and middle income sub-Saharan countries.
InEUROPEAN HEART JOURNAL 2019 Oct 1 (Vol. 40, pp. 2785-2785). GREAT CLARENDON ST, OXFORD OX2 6DP, ENGLAND: OXFORD UNIV PRESS.
Abaynew Y, Hussien M. A qualitative study on barriers to treatment and control of hypertension among patients at Dessie referral hospital, northeast Ethiopia, Ethiopia: healthcare workers’ perspective. Integrated Blood Pressure Control. 2021 Dec 3:173-8.
Lubaki JP, Mabuza L, Malete N, Ndimande JV, Maduna P. Reasons for non-compliance among patients with hypertension at Vanga Hospital, Bandundu Province, Democratic Republic of Congo: A qualitative study. African Journal of Primary Health Care and Family Medicine. 2009 Jan 1;1(1):1-5.
Pirasath S, Kumanan T, Guruparan M. A study on knowledge, awareness, and medication adherence in patients with hypertension from a tertiary care centre from Northern Sri Lanka. International Journal of Hypertension. 2017;2017(1):9656450.
Kumar Praveen N, Halesh L. Antihypertensive treatment: A study on correlates of non adherence in a tertiary care facility. Int J Biol Med Res. 2010;1(4):248- 52.
Bhandari B, Bhattarai M, Bhandari M, Ghimire A, Pokharel PK, Morisky DE. Adherence to antihypertensive medications: population based follow up in Eastern Nepal.
Hareri HA, Abebe M. Assessments of adherence to hypertension medications and associated factors among patients attending tikur anbessa specialized hospital renal unit, Addis Ababa, Ethiopia 2012. Int J Nurs Sci. 2013;3(1):1-6.
Hashmi SK, Afridi MB, Abbas K, Sajwani RA, Saleheen D, Frossard PM, Ishaq M, Ambreen A, Ahmad U. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PloS one. 2007 Mar 14;2(3):e280.
Choi HY, Lee JA, Lim J, Kim YS, Jeon TH, Cheong YS, Kim DH, Kim MC, Lee SY. Factors affecting adherence to antihypertensive medication. Korean Journal of Family Medicine. 2018 Nov;39(6):325.
Mishra S. Assessment of treatment adherence among hypertensive patients in a coastal area of Karnataka, India. International Journal of Community Medicine and Public Health. 2016 Aug;3(8):1998.
Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, Borghi C, Brignoli O, Caputi AP, Cricelli C, Mantovani LG. Adherence to
antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009 Oct 20;120(16):1598-605.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, Wainford RD. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020 Jun;75(6):1334-57.
Marin-Couture E, Moulin JA, Thibault AS, Poirier P, Després JP, Gallant A, Lamarre V, Alméras N, Lemieux I, Chabot C, Gallani MC. Impact of Lifestyle Medicine Interventions on the Management of Systemic Hypertension in Primary Care: A Canadian Randomized Controlled Trial. American Journal of Lifestyle Medicine. 2024:15598276241242013.
Hasandokht T, Farajzadegan Z, Siadat ZD, Paknahad Z, Rajati F. Lifestyle interventions for hypertension treatment among Iranian women in primary health-care settings: Results of a randomized controlled trial. Journal of research in medical sciences. 2015 Jan 1;20(1):54-61.
Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI, Chrysochoou CA, Nihoyannopoulos PI, Tousoulis DM. Dietary approaches to stop hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials. Advances in nutrition. 2020 Sep 1;11(5):1150-60.
Juraschek SP, Miller ER, Weaver CM, Appel LJ. Effects of sodium reduction and the DASH diet in relation to baseline blood pressure. Journal of the American College of Cardiology. 2017 Dec 12;70(23):2841-8.
Widmer RJ, Flammer AJ, Lerman LO, Lerman A. The Mediterranean diet, its components, and cardiovascular disease. The American journal of medicine. 2015 Mar 1;128(3):229-38.
Miller V, Mente A, Dehghan M, Rangarajan S, Zhang X, Swaminathan S, Dagenais G, Gupta R, Mohan V, Lear S, Bangdiwala SI. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): a prospective cohort study. The Lancet. 2017 Nov 4;390(10107):2037-49.
Sanuade OA, Alfa V, Yin X, Liu H, Ojo AE, Shedul GL, Ojji DB, Huffman MD, Orji IA, Okoli RC, Akor B. Stakeholder perspectives on Nigeria’s national sodium reduction program: Lessons for implementation and scale-up. PloS one. 2023 Jan 13;18(1):e0280226.
Olubodun JO, Akingbade OA, Abiola OO. Salt intake and blood pressure in Nigerian hypertensive patients. International journal of cardiology. 1997 Apr 18;59(2):185-8.
Haldar RN. Global brief on hypertension: silent killer, global public health crisis. Indian Journal of Physical Medicine and Rehabilitation. 2013 Mar 1;24(1):2-.
Bauer MS, Kirchner J. Implementation science: What is it and why should I care?. Psychiatry research. 2020 Jan 1;283:112376.