DIABETIC FOOT RISK CATEGORY ACCORDING TO INTERNATIONAL WORKING GROUP ON THE DIABETIC FOOT AMONG ADULT DIABETICS ATTENDING A TERTIARY HOSPITAL IN SOUTH-SOUTH NIGERIA
Main Article Content
Abstract
Introduction: Diabetic foot disease (DFD) constitutes a high public health burden and is a reason for hospital admission, amputation and death in persons living with diabetes mellitus. Therefore, a verified and suitable DFD classification that matches disease progression is crucial for accurate clinical diagnosis and management. This study’s objectives were to determine the prevalence of DFD and the distribution of diabetic foot risk categories according to the International Working Group on the Diabetic Foot (IWGDF) risk stratification system.
Methods: This descriptive cross-sectional study employed a simple random sampling technique to recruit 365 respondents aged 18 years or older living with diabetes mellitus. A standardised questionnaire (including the National Association of Diabetes Centres Australasian Podiatry Council foot assessment checklist and the IWGDF diabetic foot risk profile grading chart) was utilised. Data analysis was done using the IBM SPSS version 23.0.0.
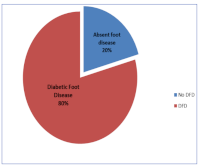
Results: The mean age of respondents was 58.35 years with S.D of 10.62 with a male to female ratio of approximately 1:1.5. Of the 365 respondents, 292 (80%) had foot disease, Using the IWGF classification, 26%, 46%, and 8% of the respondents were in category 1, 2 and 3, respectively.
Conclusion: The prevalence of diabetic foot disease among our patients was high, with more individuals classified as IWGDF diabetic foot disease category 2. This means more respondents with foot disease were at risk of getting ulcers and infections that may lead to amputation.
Downloads
Article Details
Issue
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
How to Cite
Share
References
1.Wang X, Yuan CX, Xu B, Yu Z. Diabetic foot ulcers: Classification, risk factors and management. World J Diabetes. 2022;13(12):1049–65. doi: 10.4239/wjd.v13.i12.1049
2.Mekonnen FM. Challenges of managing diabetic foot ulcers in Africa: addressing a growing healthcare crisis. J Glob Health Sci. 2024;6(1). doi:10.35500/jghs.2024.6.e8
3.Salad AM, Duale HA, Sheikh I, Gallad Dahir Hassan, Farah A, Gele A. Prevalence of diabetes foot ulcers and associated factors among adult diabetic patients in three referral hospitals in Mogadishu, Somalia. Front Public Health. 2023 ;11. doi: 10.3389/fpubh.2023.1195483
4.Abbas ZG, Boulton AJM. Diabetic foot ulcer disease in African continent: “From clinical care to implementation” – Review of diabetic foot in last 60 years – 1960 to 2020. Diabetes Res Clin Pract. 2022;183:109155. doi: 10.1016/j.diabres.2021.109155
5.Idris AO, Shamsuddin N, Hasniza ZH, Chong WL, Rehman IU. From Control to Cure: Insights into the Synergy of Glycemic and Antibiotic Management in Modulating the Severity and Outcomes of Diabetic Foot Ulcers. Int J Mol Sci. 2025 Jul 18;26(14):6909–9.
6.CDC. Diabetes Foot Problems: When to See Your Doctor [Internet]. Diabetes. 2024. [cited 2025 Dec 20]Available from: https://www.cdc.gov/diabetes/communication-resources/diabetes-foot-problems-when-to-see-your-doctor.html
7.Hu X, Zhang Y, Chen Y, Zhang YP. Validation and application of the 2019 International Working Group on the Diabetic Foot risk stratification for diabetic foot in Chinese patients. J Diabetes Investig. 2023;14(7):893–901.doi: 10.1111/jdi.14014
8.James Ngoyo Nduati, Samwel Maina Gatimu, Yeri Kombe. Diabetic Foot Risk Assessment among Patients with Type 2 Diabetes in Kenya. East Afr Health Res J. 2022;6(2):196–202. doi: 10.24248/eahrj.v6i2.698
9.Ohenhen OA, Eregie AT. Prevalence and risk factors of diabetes mellitus foot syndrome amongst persons with type 2 diabetes mellitus in a tertiary hospital in southern Nigeria. AJOL.2017;16(1):22-33.
10.Idowu AE, Amole IO, Durodola AO, Adesina SA, Idowu OA, Adegoke AO, et al. Foot-at-risk among adult outpatients with diabetes mellitus in Bowen University Teaching Hospital, Ogbomoso, Nigeria. PAMJ. 2023 Summer;46:106. doi: 10.11604/pamj.2023.46.106.39397.
11.Banik PC, Barua L, Moniruzzaman M, Mondal R, Zaman F, Ali L. Risk of diabetic foot ulcer and its associated factors among Bangladeshi subjects: a multicentric cross-sectional study. BMJ Open. 2020;10(2):034058. doi: 10.1136/bmjopen-2019-034058
12.Shaikh S, Ameer A, Saifullah S. Risk Categorization of Diabetic Foot in Patients with Type-II Diabetes and Relationship of Various Risk Factors with Risk Categories of Diabetic Foot. J Adv Med Med Res. 2020;32(23):177–8641. doi: 10.9734/jammr/2020/v32i2330732
13.Abdissa D, Adugna T, Gerema U, Dereje D. Prevalence of Diabetic Foot Ulcer and Associated Factors among Adult Diabetic Patients on Follow-Up Clinic at Jimma Medical Center, Southwest Ethiopia, 2019: An Institutional-Based Cross-Sectional Study.. J Diabetes Res 2020;2020:1–6. doi: 10.1155/2020/4106383
14.Maingi W, Kikuvi G, Matheri J. Prevalence and Factors Associated with Diabetic Foot Ulcer among Adult Patients Attending Diabetic Clinic at Nyeri Level 5 Hospital. Afr J Health Sci.2020;33(6):44–52.